As a young physician in Sydney, Australia in 1979, Colin Sullivan conceived of an experiment to help people with nighttime breathing issues. After several months of waiting for the right patient, he met a construction worker so tired from disrupted overnight sleep that he habitually dozed off on the scaffolding.
The man had sleep apnea—his airway was obstructed, which interrupted breathing at night, waking him repeatedly. But he refused Sullivan’s recommendation for surgery to create an opening in the neck, the only known treatment back then.
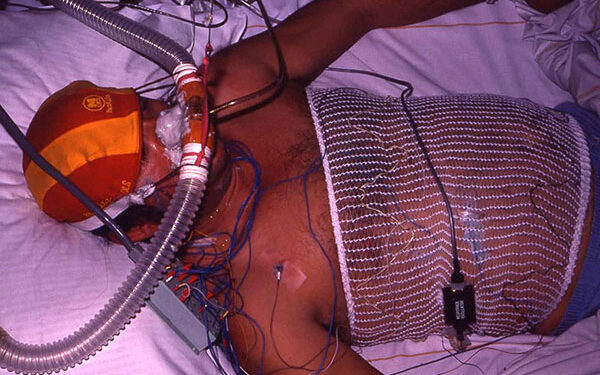
The day had come for Sullivan to try a contraption he’d invented, a “big swimming pool pipe attached to a blower,” as he describes it. Through a mask, the device delivered air into the man’s nose, creating a slight increase in pressure that kept his airway open. He slept peacefully for the first time in years.
“It was an amazing result,” Sullivan says. At the time, though, he “never imagined” there’d be such a need for his continuous positive airway pressure, or CPAP machine. Rates of obesity, a major driver of sleep apnea, had just begun to rise. In today’s obesity epidemic, nearly a billion people worldwide have sleep apnea.
CPAP machines, Sullivan soon learned, have their limits. “Many people can’t use them,” he says. “There’s a lot of individuality with sleep apnea.” Advances are helping people use CPAP more effectively and providing alternatives. Here are the most promising approaches, according to experts.

Sleep apnea and CPAP
Although CPAP machines work well for tens of millions, many other people struggle with them. Some of these challenges can be addressed with the right guidance and strategies.
“I’ve used CPAP for 16 years, and I never felt really well-rested,” says Emma Cooksey, a patient advocate at the nonprofit Project Sleep. One problem for Cooksey, often experienced by others, was a poorly fitting mask. The machine was handed to her without any instructions on troubleshooting comfort issues. “Figuring out how to get comfortable with CPAP is a big missing part of the process,” she says.
“It’s not one-size-fits-all,” says Dr. Kevin Motz, an ear-nose-throat (ENT) physician and sleep apnea researcher at Johns Hopkins. Nose-only masks are generally most effective, but masks that extend over the mouth can benefit those who struggle with nasal breathing. Searching through thousands of available masks can be overwhelming without support and supervision from knowledgeable respiratory therapists and medical equipment companies. However, “access to these experts is often limited,” Motz says.
Read More: Why Do Some People Need More Sleep Than Others?
Within a few years of starting CPAP, about 50% of patients use it too infrequently or stop completely. Left untreated, sleep apnea contributes to serious health issues including heart disease, strokes, and diabetes.
Cloud-based platforms and several apps help engage people in using CPAP, and some telehealth companies specialize in providing expertise virtually to fit people with the best mask. Examples are Lofta and Better Night. Accessories can make CPAPs more usable, such as snug cushion covers and stands that hold the CPAP hose above the head and out of the way. A chin strap to keep the mouth closed is another strategy shown to improve tolerance for CPAP, Motz says.
Another approach is working with a cognitive behavioral therapist to address insomnia symptoms, claustrophobia, or anxiety posed by CPAP.
Sometimes airways are obstructed at least partly due to certain facial and oral structures, like a recessed jaw or large tongue, that make it harder for CPAP alone to open the airway enough, even if the mask fits well, Motz says. Less common than obstructive sleep apnea is another form called central sleep apnea, in which breathing muscles aren’t active enough. For these patients, CPAP may not help as much.
Getting the right diagnosis
Another challenge is simply knowing which group you fall into. It’s sometimes unclear what’s causing sleep apnea or even whether you have it in the first place. An accurate diagnosis is key to finding the right solution.
One sign of sleep apnea is whether you snore. “Snoring is part of the problem” and should be checked out with doctors, says Sullivan, now an emeritus professor of medicine at the University of Sydney.
Commercial sleep trackers in watches and beds can support detection. Researchers are studying the reliability of these sensors, but if they provide a sleep apnea alert, follow up with your doctor and a sleep specialist, Motz says. They might recommend a comprehensive sleep study to find out more.
Read More: Sleep Doctors Share the 1 Tip That’s Changed Their Lives
Another type of exam is a sleep endoscopy, where a tiny camera is inserted down the airway to find specific places where it’s obstructed. This can lead to more individualized treatment options. ENT doctors know about and recommend sleep endoscopies in certain situations. Otherwise, it’s “not commonly available to people,” Cooksey says.

New medications
About 20 years after Sullivan’s CPAP discovery, Dr. Atul Malhotra began his career as a sleep apnea researcher. “I vowed to find new treatments,” says Malhotra, a sleep medicine specialist and vice chair of medicine for research at UC San Diego. “Not for lack of trying, it took me 25 years. But now we have one.”
He’s referring to one of the new GLP-1 weight loss medications, called tirzepatide. It helps some people with sleep apnea, according to Malhotra’s 2024 study. Malhotra, who’s also a sleep medicine specialist at UC San Diego Health, thinks the drug works mainly through weight loss, which reduces fat blocking the airway.
His study focused on people with obesity, and it was funded by Eli Lilly, the manufacturer of tirzepatide. More research is needed to understand its effects. Malhotra adds that if you stop taking this drug, the weight tends to come back. Plus, it’s expensive. “Our goal was to complement CPAP, not replace it,” he says. “These therapies often go hand-in-hand.”
Read More: How to Get Your Partner to Stop Snoring
Several other drugs are being studied. One, a potassium channel antagonist, is taken as a nasal spray and improved apneas in a small trial this year. It activates muscles that widen the throat to improve airflow, says the study’s co-author, Danny Eckert, professor and director of sleep health at Flinders University and a part-time investigator at the Brigham and Women’s Hospital. Another drug, called atomoxetine, also affects muscles in ways that could help, according to recent studies.
We don’t know the long-term effects of these medications, Eckert points out. Sullivan, with his 50-year window on sleep apnea research, recalls progesterone, a steroid that seemed to show benefits for sleep apnea in the 80s—before it was found to raise blood pressure.
Lifestyle
While drug research continues, lifestyle behaviors can help right now. For many people, reducing weight through exercise and healthy nutrition is a powerful strategy to counter sleep apnea.
“If your weight goes up, you’re fighting an uphill battle,” Motz says. Dropping 10-15% can reduce sleep apnea severity by about 50%.
Aim for conventional exercise to support weight loss—or more targeted activity. Speech pathologists can lead you through exercises of the throat, called myofunctional therapy, that may increase the endurance of airway muscles, Eckert says, benefiting sleep apnea. Alternatively, a device called eXciteOSA can work these muscles through electrical stimulation.
Eckert has also found a link between healthy, plant-based diets and 20-30% lower risk of developing sleep apnea. In addition to keeping off the pounds, plant-centric diets lower inflammation throughout the body, another driver of sleep apnea, Eckert says.
But exhaustion from poor sleep increases hunger hormones, intensifying food cravings, Cooksey notes. Sleep apnea drained her energy so much that she left a career in law, opting for less demanding administrative jobs. Four years ago, she started interviewing experts for a podcast to better understand treatments for the disorder.
In addition to nutrition and exercise, she’s come to appreciate the importance of sleep hygiene, such as getting natural daylight in the morning. The right sleep position is important because sleeping on your back can worsen the problem. “Our sleep hygiene has to be even better than the rest of the population,” Cooksey says.
Surgery
Surgery is sometimes another option. Often, this means removing or rebuilding tissues of the airway. Two decades ago, surgeons had no way of knowing which part to cut, Motz says, but he and others have developed more precise methods. Pre-surgery, they perform a sleep endoscopy (the procedure involving the camera), to see exactly how the person’s airway is collapsing. “That helps us tailor the surgical treatment to the patient,” Motz says.
In another type of operation, surgeons implant a device into the chest that connects to an electrode in the neck, which stimulates a nerve that controls the tongue. Called an Inspire implant, this device sends gentle pulses overnight that move the tongue forward, opening the airway. The implant can help considerably, though researchers are working to improve it.
“We know surgery isn’t always effective,” Motz says. Because it’s invasive, surgery is appropriate only for moderate or severe cases; Motz recommends patients try CPAP and other treatments first. He explores a variety of solutions at his clinic.
Oral devices
Many people with sleep apnea benefit from oral devices that pull the lower jaw forward and hold it there, enlarging the opening at the back of the throat. “Oral devices can be quite effective,” sometimes when combined with CPAP, Sullivan says.
These aren’t just run-of-the-mill mouthguards, and getting a dentist to personalize one to your mouth can be challenging. Most dentists have little background on sleep apnea. It’s necessary to find a dentist trained and certified as an expert in dental sleep medicine.
Read More: How to Get Back to Sleep After Waking Up at Night
Recently, Cooksey worked with her sleep specialist and a trained dentist to fit a custom oral device. She also organized a sleep study to observe its effects, with most of the coordination falling on her. Sleep apnea involves multiple specialists who “work in silos and don’t talk to each other,” she says.
Other options on the horizon
After Cooksey combined CPAP with the oral appliance, her sleep apnea improved along with her daytime energy. Finding the right solution required trial-and-error with myriad strategies that work for some, but didn’t pan out for her. “We need as many options as possible,” she says.
More alternatives are on the way. For example, Eckert is working to improve the potassium channel blockers. “Cool innovations are happening,” he says. “This whole area is going to spread wide open in the next 5-10 years.”
These innovations will likely be combined with older ones, Sullivan says. “After all these years, I’ve been expecting a cure from surgery or drugs, but it hasn’t happened,” he says. “I think CPAP will maintain a very important role.”